A new variant of coronavirus has spread across the United Kingdom and has been detected in the United States, Canada and elsewhere. Scientists are worried that these new strains may spread more easily.
As an evolutionary biologist, I study how mutation and selection combine to shape population changes over time. We have never had so much real-time data on evolution as in the case of SARS-CoV-2: over 380,000 genomes were sequenced last year.
SARS-CoV-2 was mutant as it spread, causing slight differences in its genome. These mutations allow scientists to track who is related to who in the virus’s family tree.
Evolutionary biologists, myself included, have warned against overinterpreting the threat posed by mutations. Most mutations will not help the virus, just as random hitting a work machine is unlikely to improve it.
But from time to time, a mutation or a series of mutations gives the virus an advantage. The data are convincing that the mutations brought about by the variant that first appeared in the United Kingdom, known as B.1.1.7, make the virus more “appropriate”.
Fitness or higher chance?
When a new variant becomes commonplace, scientists determine why it has spread. A virus that carries a certain mutation can increase in frequency by chance if it is:
- worn by a superspreader;
- moved to a new uninfected location;
- introduced into a new segment of the population.
The last two examples are called “founding events”: a rapid increase in frequency can occur if a particular variant is introduced into a new group and triggers a local epidemic. Random events may explain the increase in the frequency of several different SARS-CoV-2 variants.
But B.1.1.7 is an exception. It shows a very strong selection signal. In the last two months, B.1.1.7 has grown in frequency faster than non-B.1.1.7 practically every week and health region in England. These data, reported on 21 December 2020, helped persuade British Prime Minister Boris Johnson to place much of the country under lockdown and led to widespread travel bans in the UK.
Spreading B.1.1.7 through England in November and December, with the London insert at the top right. pic.twitter.com/fVfL0xijcx
– Theo Sanderson (@theosanderson) January 8, 2021
The increase in B.1.1.7 cannot be explained by a founding event in new regions, as COVID-19 is already circulating in the UK Founder events in a new segment of the population (eg following a conference) also do not are plausible given the widespread restrictions against large assemblies at that time.
Our ability to track the evolution of SARS-CoV-2 is due to the massive effort of scientists to share and analyze data in real time. But the incredibly detailed knowledge we have about B.1.1.7 is also due to simple luck. One of its mutations altered a section of the genome used to test COVID-19 in the UK, allowing the image of the evolutionary spread to be extracted from more than 275,000 cases.
Evolution in action
Epidemiologists have concluded that B.1.1.7 is more transmissible, but there is no evidence that it is more lethal. Some researchers estimate that B.1.1.7 increases the number of new cases caused by an infected person (called the reproduction number or Rt) by between 40 and 80%; another preliminary study found that Rt increased by 50-74 percent.
A 40-80% advantage means that B.1.1.7 is not only slightly more suitable, it is much more suitable. Even when the selection is so strong, the evolution is not instantaneous. Our mathematical modeling, as well as that of others in Canada and the USA, shows that it takes B.1.1.7 a few months to reach meteoric growth, because only a small part of the cases initially carry the new variant.
For many countries, such as the USA and Canada, where the number of COVID-19 cases has increased precariously, a variant that increases the transmission by 40-80% threatens to push us over. It could lead to an exponential increase in cases and overwhelm the already thin healthcare. Evolutionary changes take some time, buying us maybe a few weeks to prepare.
More options
A surprise for researchers was that B.1.1.7 carries a remarkable number of new mutations. B.1.1.7 has accumulated 30-35 changes in the last year. B.1.1.7 is not moving at a faster pace, but it seems to have undergone a rapid change in the recent past.
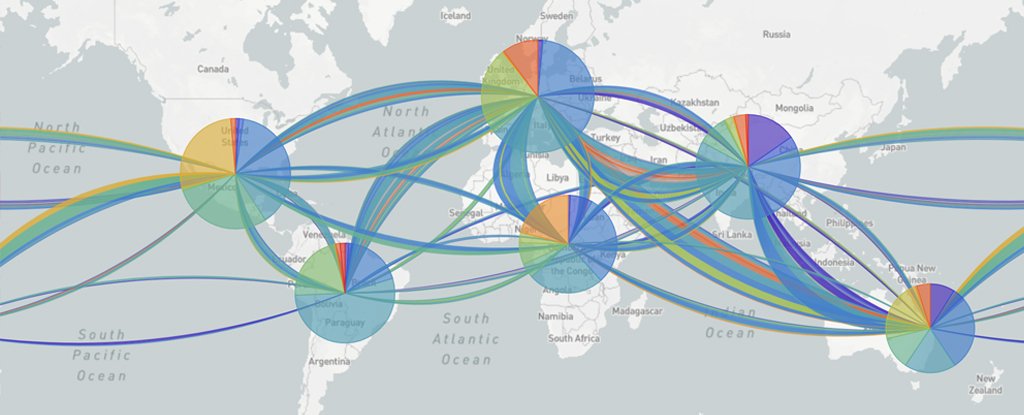
 (NextStrain / CC BY 4.0)
(NextStrain / CC BY 4.0)
The virus may have been carried by an immunocompromised person. People with weaker immune systems are constantly fighting the virus, with prolonged infections, recurrent rounds of viral replication and only a partial immune response to which the virus is constantly evolving.
Preliminary research reports that have not yet been verified have described two other options of concern: one from South Africa (B.1.351) and one from Brazil (P1). Both variants show a recent history of excess mutations and rapid increases in frequency in local populations. Scientists are currently collecting the data needed to confirm that selection for higher transmission, not chance, is responsible.
What has changed to allow it to spread?
Selection plays two roles in the evolution of these variants. First consider the role in those individuals in which the large number of mutants appeared. 23 mutations of B.1.1.7 and 21 mutations of P1 are not randomly distributed in the genome, but are grouped in the gene encoding the spike protein.
A tip change, called N501Y, occurred independently in all three variants, as well as in immunocompromised patients studied in the US and the UK. Other peak changes (e.g., E484K, del69-70) are observed in two of the three variants.
Beyond the peak, the three variants of concern share an additional mutation that eliminates a small part of the so-called “nonstructural protein 6” (NSP6). We don’t know yet what deletion does, but in a related coronavirus NSP6 fools a cellular defense system and can promote coronavirus infection. NSP6 also hijacks this system to help copy the viral genome. Either way, deletion could alter the virus’s ability to seize and replicate in our cells.
Easier transmission
The parallel evolution of the same mutations in different countries and in different immunocompromised patients suggests that they transmit a selective advantage to evade the immune system of the individuals in which the mutations occurred. For N501Y, this was supported by experiments in mice.
But what does the higher individual-to-individual transmission rate matter? This is difficult to answer, as the many mutations that have occurred simultaneously are now grouped in these variants and could be any or a combination of them that would lead to the advantage of transmission.
That being said, many of these variants have previously appeared on their own and have not led to rapid spread. One study showed that N501Y had a weak transmission advantage on its own, increasing rapidly only when associated with the suite of mutations observed in B.1.1.7.
While the evolutionary story of COVID is still being written, an important message is now emerging. The 40-80% transmission advantage of B.1.1.7 and, potentially, the other variants B.1.351 and P1, will overwhelm many countries in the next few months.
We are in a race against viral evolution. We need to launch the vaccines as soon as possible, stop the flow of variants by restricting interactions and travel, and get ahead of the spread by stepping up surveillance and tracking of contacts. ![]()
Sarah Otto, Killam Professor of Evolutionary Biology, University of British Columbia.
This article is republished from Conversation under a Creative Commons license. Read the original article.