Some infectious bacteria have adapted so well to the human bladder that they appear to make their own DNA using chemicals in our urine.
The urinary tract is a difficult place for most bacteria to survive. Therefore, it is often said that urine is sterile, although this is not true.
Like your gut, human urine hosts a community of microbes, known as the microbiota, and although most bacteria that live inside it are harmless, sometimes a certain species can tip the scales, causing painful urinary tract infections (UTIs).
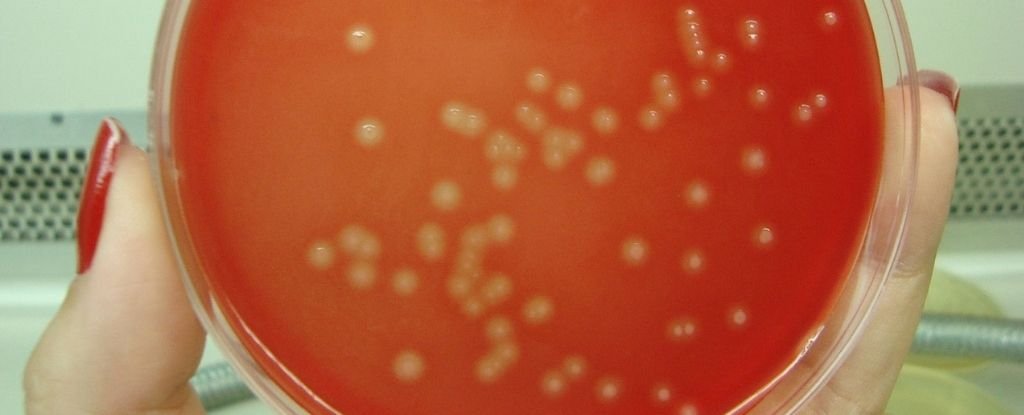
Streptococcus agalactiae it is a well-known source of ITU in some people, and new research has now revealed how it can survive in such an unfriendly environment.
In a healthy human body, urine must be relatively low in the four nucleobases that make up the DNA code, which are broken down into nitrogenous and excreted compounds.
Sequencing S. agalactiae genome, scientists have now found a key, specialized gene that allows the bacterium to exploit the presence of other compounds in the urine to produce at least one of these bases – guanine – for it to survive.
Similar genes have also been found recently in Escherichia coli (E. coli), which is the most common offender of human ITU.
Usually in the gut or blood, And there and streptococcal removes certain chemicals they need to produce DNA, borrowing products like guanine from our own bodies. However, in the urinary tract, these essentials are eventually broken down into uric acid, which means they are not as easy to find.
It is a difficult situation and it means both And there and streptococcal they must synthesize their own chemical bases if they want to grow and reproduce.
“It’s basically a survival strategy to colonize urine, an environment where many organisms can’t live,” explains molecular geneticist Matthew Sullivan of Griffith University in Australia.
It seems to be a common strategy among the species of bacteria that make up the urine microbiome.
In the study, scientists used mice to show how essential this specialized gene, known as guaA, really is. Collection streptococcal strains from several individuals, the researchers compared a normal S. agalactiae infection with a form of guaA-deficient bacterium.
Microbes that could not create their own guanine failed to colonize the bladder of mice to the same extent. The same thing was found when the researchers used synthetic human urine.
This suggests that guaA is essential for a streptococcal the infection to catch in the bladder, not only in mice, but also in us.
When the researchers added extra guanine to the urine, even bacterial strains without metabolic pathways to create guanine on their own managed to survive and thrive, suggesting that this basis is a key limiting factor.
Compared to And there, streptococcal shows key differences in how it controls guaA genes, but the results seem quite similar and give us a new way to treat UTIs, which have become increasingly resistant to available antibiotics.
Already, techniques aimed at synthesizing guanine in other parts of the body have helped combat other forms of streptococcal bacteria.
Although not as common as And there bladder infections, streptococcal causes about 160,000 ICUs each year in the US, and these can be difficult to treat, especially since we don’t know much about how the infection works.
Moreover, because streptococcal UTIs often occur in pregnant and elderly people and in patients with underlying health conditions such as diabetes, finding safe and effective treatment options becomes even more difficult.
“Such research gives us new opportunities to develop alternative treatments in a world of high antibiotic resistance due to overuse of existing drugs. For example, we could target this path in efforts to design new drugs to prevent infection.” , Sullivan explains.
“Overall, the study illustrates the importance of fundamental findings that help us perceive how microorganisms interact with humans.”
The study was published in Journal of the International Society of Microbial Ecology (ISME).