
Fecal transplants, already being studied as a treatment for colon infections and type 2 diabetes, may also help the body fight cancer, new research funded by the US government suggests. In a small clinical trial, some advanced cancer patients who received transplants began to respond to treatments that did not work earlier, which either stabilized them or reduced their tumors.
The purpose of a fecal transplant is to use a donor’s stool to reset a person’s intestinal microbiome, the vicinity of bacteria that live along our digestive tract. The intestinal microbiome helps the body regulate everything from metabolism to a properly functioning immune system, and an unbalanced microbiome is believed to cause or increase the risk of many health problems, such as diabetes, inflammatory bowel disease and certain infections. By inoculating the digestive tract with bacteria from the donor’s stool, it seems possible to grow a healthier intestinal microbiome.
Currently, fecal microbiota transplantation (FMT) is considered only an effective treatment for recurrent gastrointestinal infections caused by Clostridioides difficult, which can be fatal. But there are ongoing studies testing its use for other conditions. This new study was led by researchers at the University of Pittsburgh Medical Center Hillman Cancer Center, as well as scientists from National Cancer Institute. They looked at FMT as a kind of booster for another emerging treatment, cancer immunotherapy.
Immunotherapy uses drugs to boost the immune system’s ability to find and destroy cancer cells. These drugs include immune checkpoint inhibitors, which eliminate the natural limiter that some cancers use to avoid detection by T cells. Although immune checkpoint inhibitors have shown great promise in treating advanced cancers, tumors some people continue to resist the suppression of the immune system even after treatment. Some researchers theorized that resetting the intestinal microbiome of these patients will make these tumors vulnerable to immunotherapy.
G / O Media may receive a commission
“Cancer therapies are often based on stimulating anti-tumor immune responses, increasing the likelihood that the gut microbiota will influence host responses to cancer treatments through the immune system,” said study author Giorgio Trinchieri, head of the NCI Integrative Cancer Immunology Laboratory. for Cancer Research, Gizmodo said in an email.
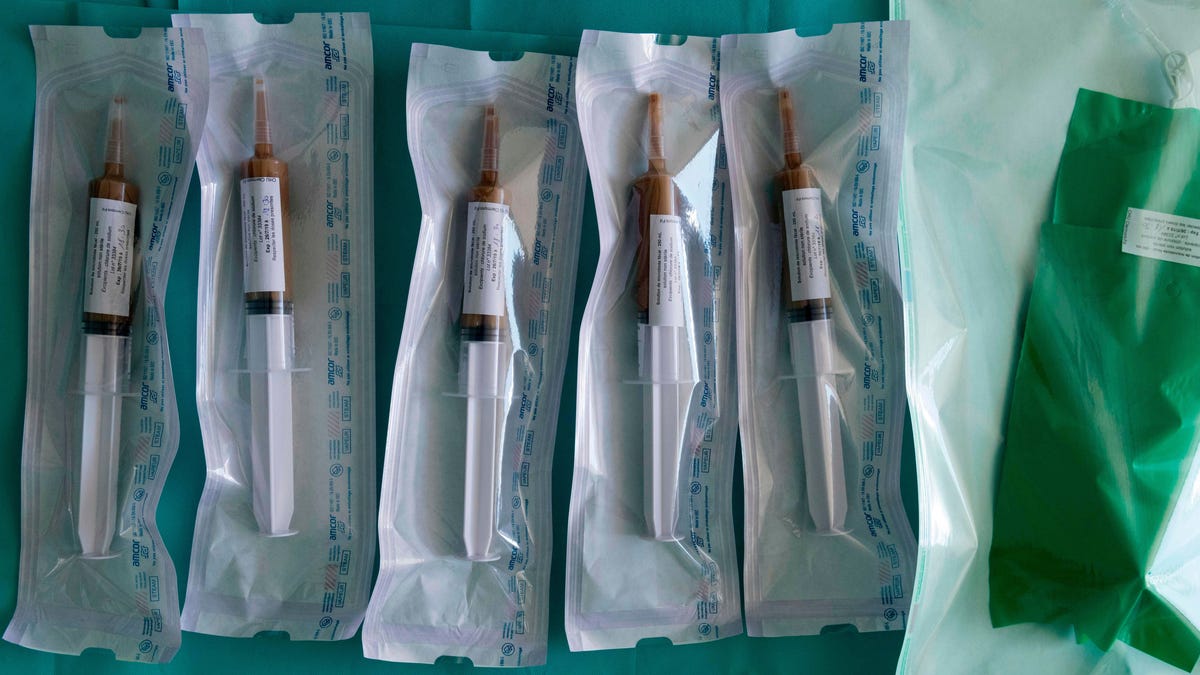
UPMC researchers treated 15 patients with advanced melanoma, the deadliest form of skin cancer, who had not previously responded to treatment with immune checkpoint inhibitors. These patients received transplants from other patients with advanced melanoma who responded to therapy (often patients receive a dose of antibiotics first to help clarify their existing microbiome, but not in this study). The donor seat was examined for potentially dangerous germs – a precautionary measure that has become standard in wake up in several diseases and a death related to fecal transplants carrying drug-resistant bacteria in 2019. NCI assisted in the analysis of microbiome samples from these patients.
Subsequently, six of the 15 patients began to respond to treatment. In one patient, their tumors continued to shrink for more than two years and in numbers, while four others had stabilized cancer with no signs of disease progression for at least a year. (The sixth patient appeared to respond fully to immunotherapy, but died shortly after treatment due to complications from unrelated surgery.)
In these patients, the tumor progresses rapidly and life expectancy has been short, Trinchieri noted. “Stable disease and tumor contraction would significantly improve patients’ survival and quality of life and could lead to long-term survival and, in some cases, healing.”
Both the intestinal microbiome and the immune system of these patients also showed signs that they changed favorably after transplantation, allowing a better response to therapy. Transplants themselves were also well tolerated, although immunotherapy probably caused minor side effects in some patients, including fatigue. finding were published in the journal Science on Thursday.
The study, according to Trinchieri, is one of the first to show that changing the gut microbiome can improve a person’s response to immunotherapy. And while this is just a proof-of-concept study, it also demonstrates the potential to target the microbiome in general for cancer treatment.
Despite this potential, more work needs to be done with larger groups of patients before poop transplants can become a standard of care for difficult cancers. The team’s research and others are beginning to identify the types of bacteria that could improve the response to immunotherapy, as well as the patients most at risk for a transplant. I also keep track of patients who have responded to FMT, while using their donated poop for other studies.
In the future, this transplant technique – which requires a colonoscopy – may not even be the preferred method of delivery. Instead, Trinchieri said, maybe we could only get it by using a pill that contains bacteria. Fortunately, some studies are already exploring this method, as well as the use of FMT for other cancers.
This article was updated to note that researchers at the UPMC Hillman Cancer Center played a major role in this study, including in the treatment of these patients.